Introduction
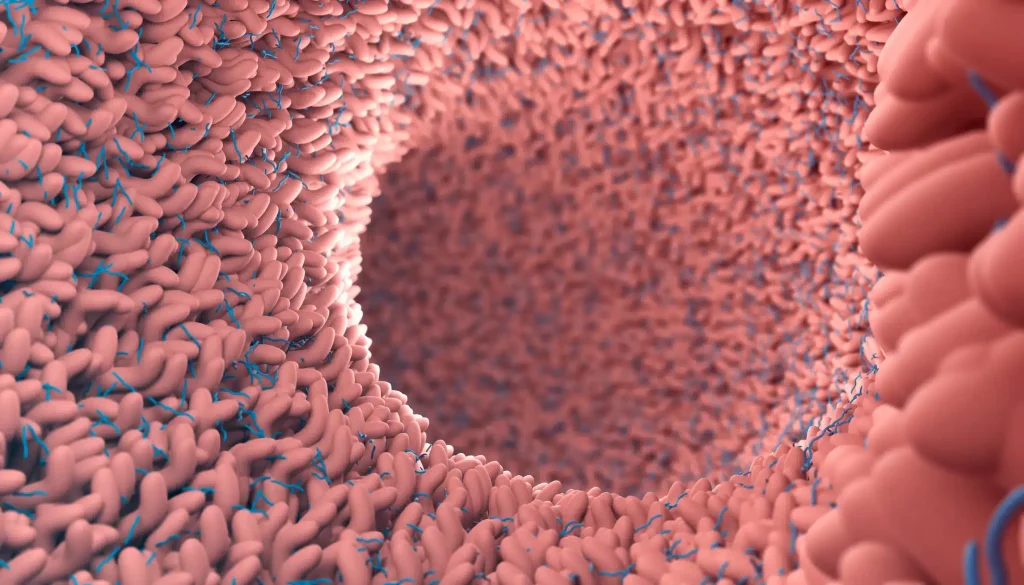
Chronic intractable diarrhea remains a diagnostic challenge for many patients despite detailed evaluations. Traditional biopsies often appear unremarkable, yet a closer examination of mucosal mast cells reveals significant insights.
Mast Cell Concentration in Chronic Diarrhea
In this study, we examined the concentration of mast cells in colonic or duodenal biopsy specimens from 47 patients with chronic intractable diarrhea. Immunohistochemical analysis for mast cell tryptase was used, comparing results to those from 50 control subjects and 63 patients with other chronic diarrhea diseases, such as inflammatory bowel disease and celiac disease.
Findings
The control group showed an average of 13.3 mast cells per high-power field. In contrast, 33 out of 47 patients with chronic intractable diarrhea had more than 20 mast cells per high-power field. Notably, 67% of these patients experienced symptom relief through drugs affecting mast cell function, such as H1 and H2 receptor antagonists and mast cell mediator release inhibitors.
Mastocytic Enterocolitis: A Novel Diagnosis
The term “mastocytic enterocolitis” has been coined to describe this condition, characterized by increased mucosal mast cells demonstrated through immunohistochemistry. This is distinct from systemic or cutaneous mastocytosis and is not evident in other chronic diarrhea diseases. The increased mast cells are reactive and specific to the gut mucosa, suggesting a gut-specific phenomenon driven by unknown stimuli.
Clinical Implications
Mast cells play a crucial role in regulating intestinal sensory and motor functions, potentially causing diarrhea and abdominal pain through their mediator release. This study emphasizes the importance of considering mast cell function in chronic intractable diarrhea cases, as traditional evaluations might miss this significant factor.
Conclusion
Mastocytic enterocolitis should be considered in patients with chronic intractable diarrhea when routine biopsies appear normal. Immunohistochemical staining for mast cell tryptase can reveal increased mast cells, guiding effective treatment options. Further research is essential to understand the triggers and mechanisms behind this condition.
Visit our resources for more articles.