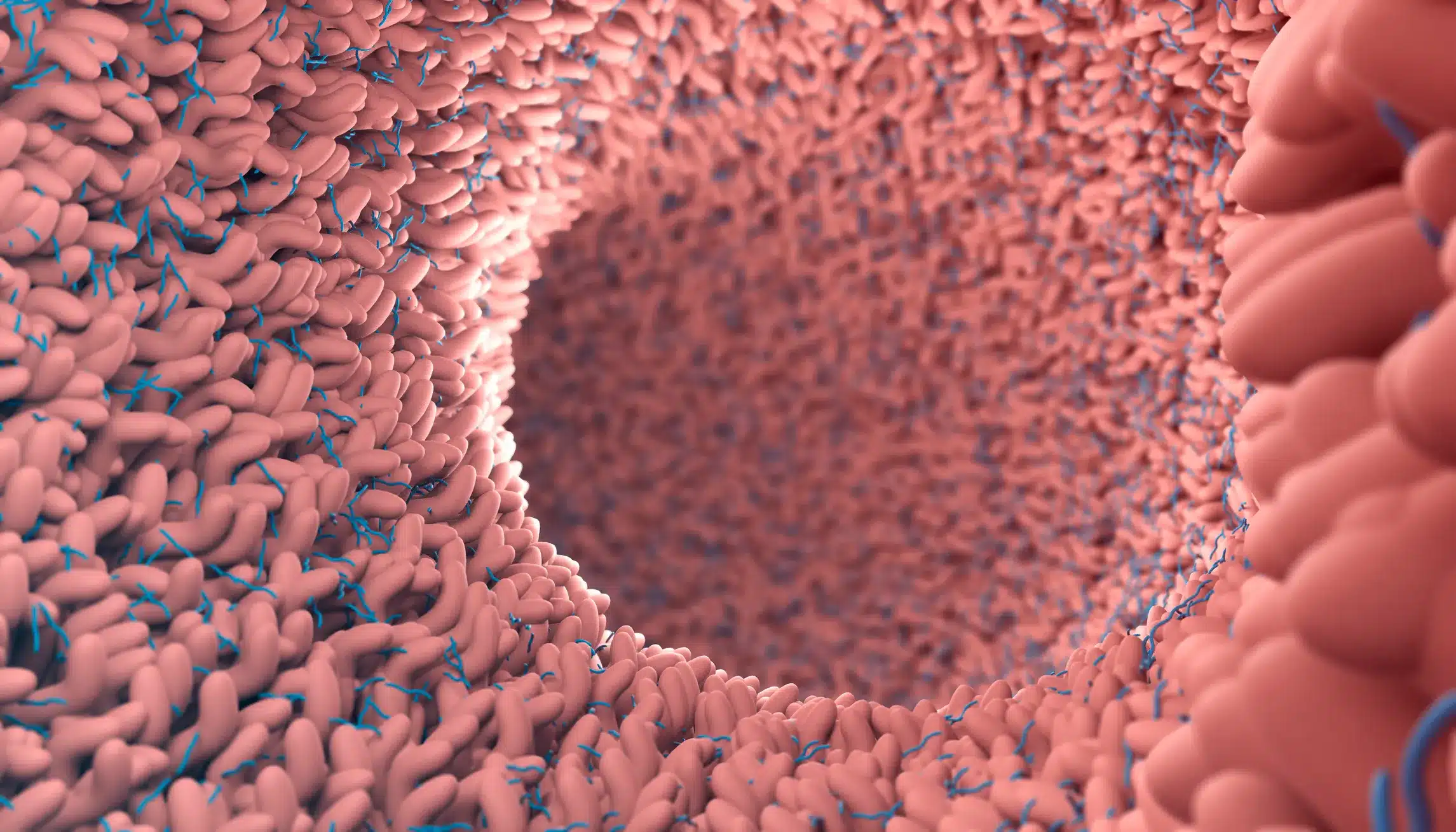
Acute diarrheal infections are a pervasive health issue affecting millions of people each year, leading to significant healthcare costs and impacting quality of life. These infections, caused by various pathogens, are common both domestically and among international travelers. To address this issue, the American College of Gastroenterology (ACG) has developed comprehensive, evidence-based guidelines focusing on the diagnosis, treatment, and prevention of acute diarrheal infections in immune-competent adults.
Epidemiology and Public Health
Acute diarrheal infections are a leading cause of outpatient visits and hospitalizations in the United States, significantly impacting public health. Risk factors include consuming contaminated food or water, traveling to high-risk areas, and person-to-person transmission. Surveillance and outbreak investigations are crucial in controlling the spread.
Diagnosis Guidelines
Proper diagnosis is essential, especially in severe cases, instances of dysentery, or when symptoms persist beyond seven days. Traditional methods like bacterial cultures, microscopy, and antigen testing are useful, but the ACG recommends incorporating FDA-approved culture-independent methods for more accurate pathogen identification and effective treatment.
Effective Treatment Strategies
Oral rehydration with balanced electrolyte solutions is vital, especially for severe cases and travelers with cholera-like diarrhea. This method ensures that fluid and electrolyte losses are adequately replaced, preventing dehydration. Antibiotic therapy is advised for severe infections, travel-related cases, or when specific bacterial pathogens are identified. Probiotics and prebiotics are generally not recommended for treating acute diarrhea in adults, except in post-antibiotic cases.
Symptom Management with Bismuth Subsalicylates and Loperamide
Bismuth subsalicylates (BSS) and loperamide are effective non-antibiotic options for managing symptoms. BSS can reduce stool frequency, improving patient comfort during illness. Loperamide, particularly when used with antibiotics for traveler’s diarrhea, helps shorten the duration of diarrhea and increases the likelihood of a cure.
Preventive Measures
Prevention is crucial in managing acute diarrheal infections. Pre-travel counseling on avoiding high-risk foods and beverages is essential for travelers. Strict hand hygiene and cautious food and water intake are important preventive steps. In specific scenarios, like cruise ship outbreaks or institutional settings, frequent hand washing and alcohol-based hand sanitizers can be beneficial. Bismuth subsalicylates may offer additional protection for travelers without contraindications.
Key Recommendations
- Diagnostic Testing: Conduct stool tests in severe or persistent cases and during outbreaks.
- Oral Rehydration: Use balanced electrolyte solutions to treat severe diarrhea and prevent dehydration.
- Antibiotic Therapy: Reserve antibiotics for severe infections, travel-related cases, or specific bacterial pathogens.
- Symptom Control: Use BSS and loperamide to reduce symptoms and improve comfort.
- Preventive Practices: Emphasize hand hygiene, safe food and water practices, and consider BSS for travelers.
Conclusion
Acute diarrheal infections require a comprehensive approach to diagnosis, treatment, and prevention. By following the ACG’s guidelines, healthcare providers can effectively manage these infections, reducing their impact on patients and public health. Emphasizing preventive measures, appropriate diagnostic testing, and effective treatment options are key strategies in combating acute diarrheal infections in adults.
Visit our resources for more articles.